U.S. Revenue Cycle Management Industry Overview
The U.S. Revenue Cycle Management Market, valued at approximately $172.24 billion in 2024, is projected to grow at a CAGR of 10.1% from 2025 to 2030. The swiftly evolving healthcare landscape, marked by increasing digitalization, has created opportunities for the adoption of healthcare IT services, including revenue cycle management (RCM) systems. These systems aim to organize and streamline healthcare organization workflows through synchronized management software solutions. RCM solutions integrate payment models, reimbursement guidelines, codes, and interactions with third-party payers. The complexities inherent in billing and ensuring accurate payment for medical services are anticipated to drive the demand for innovative RCM solutions.
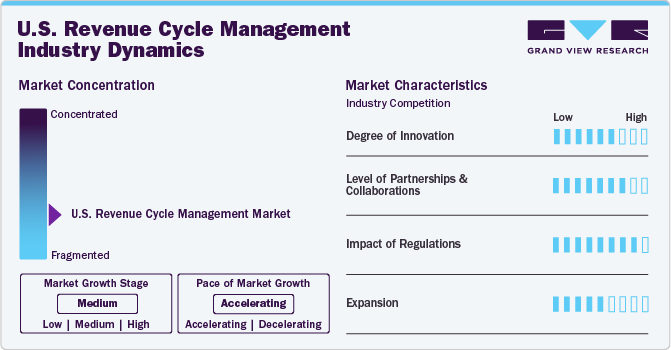
The practice of U.S. healthcare entities outsourcing RCM is gaining momentum due to its increasing advantages. The market is expected to experience substantial growth as a result of the intricate and labor-intensive nature of RCM processes, a shortage of qualified healthcare professionals, the necessity for cost-effective solutions, and the challenges presented by strict regulations, financial constraints, and staff shortages within the healthcare sector. Consequently, healthcare providers are increasingly choosing to outsource RCM tasks to specialized companies to optimize processes, decrease expenses, enhance accuracy, and prioritize patient care over administrative duties. This trend is likely to persist as providers seek efficient cash flow, cost reductions, and improved value-based care delivery.
Detailed Segmentation:
- Component Insights
The software segment is anticipated to grow significantly during the forecast period, owing to a growing demand for digitalization and streamlining of operational workflows to improve patient care. The growing amount of unorganized data generated from multiple healthcare functionalities requires centralization and consolidation, which is anticipated to drive the software segment over the forecast period.
- Product Insights
The integrated segment dominated the market in 2024 with a market share of over 71.84% and is anticipated to grow at the fastest rate during the forecast period. This is attributed to the constant technological advancements and rapid adoption of integrated RCM solutions by healthcare organizations. Furthermore, integrated solutions provide a synchronized and streamlined platform for financial activities with a standardized data collection and analysis process, which is expected to drive the market over the forecast period.
- Delivery Mode Insights
The web-based segment dominated the market in 2024 with a market share of over 56.76%. Web-based solutions are being increasingly implemented since these solutions are to be installed off-site and do not require additional hardware or storage. Affordability and rapid deployment are some of the benefits offered by web-based solutions. athernaOne, e-Hospital Systems, Simplex HIMES, and Advanced HIMS are examples of web-based practice management solutions. The cloud-based segment is anticipated to grow at the fastest rate during the forecast period.
- Specialty Insights
The cardiology segment held a significant share of 7.15% in 2024 and is expected to grow at the fastest rate during the forecast period. Cardiology treatments are expensive procedures requiring RCM services; these services help enhance the procedure's effectiveness & patient care and seamlessly manage medical billing. According to an Elsevier, Inc. paper in September 2023, approximately 6.7 million U.S. adults aged 20 years and above had heart failure, and the prevalence is projected to reach 8.5 million by 2030. The rising prevalence of cardiovascular diseases directly increases the workload burden on healthcare providers and healthcare payers, which is expected to drive the segment.
- Sourcing Insights
The in-house segment dominated the market in 2024 and accounted for a revenue share of over 70.82%. The segment growth is attributed to associated benefits, such as complete control of coding operations, patient information confidentiality, and accessibility of in-house medical billers. One of the major challenges in-house RCM services face is the requirement of a large medical staff to handle the patient’s medical data. Healthcare providers need to employ trained billers and coders, which can result in backlogs if one of them is ineffective, jeopardizing the entire revenue cycle.
- End-use Insights
The hospitals segment is expected to grow at the fastest rate during the forecast period. This is attributed to the growing presence of renowned and well-established hospitals in the U.S. and the rising number of patient care regulatory reforms & guidelines introduced by regulatory agencies. Hospitals are focusing on implementing innovative RCM solutions by collaborating with vendors to transform the reimbursement scenario, which is anticipated to boost segment growth. Moreover, the growing demand to optimize hospitals’ workflow to improve efficiency and productivity is expected to boost the adoption of integrated RCM systems in hospitals.
- Function Insights
The claims management segment dominated the market in 2024 with a market share of over 52.78%. This is attributed to the swiftly expanding patient pool, the rising geriatric population, and the introduction of advantageous government programs related to medical insurance coverage. In addition, the adoption of risk- or value-based reimbursement models is boosting the implementation of enhanced supervision and revenue cycle prediction, particularly for high-risk & vulnerable patient groups.
Gather more insights about the market drivers, restraints, and growth of the U.S. Revenue Cycle Management Market
Key Companies & Market Share Insights
Some emerging companies in the market are Aidéo Technologies, Access Healthcare, TELCOR, CorroHealth, and others. Key players' strategies to strengthen their market presence include new product launches, partnerships & collaborations, mergers & acquisitions, and geographical expansion.
Key U.S. Revenue Cycle Management Companies:
- athenahealth, Inc.
- Cerner Corporation
- eClinicalWorks
- Epic Systems Corporation
- McKesson Corporation
- NXGN Management, LLC
- Oncospark, Inc.
- R1 RCM, Inc.
- The SSI Group, Inc.
- Veradigm LLC (Allscripts Healthcare LLC)
Order a free sample PDF of the Market Intelligence Study, published by Grand View Research.
Recent Developments
- In January 2025, Access Healthcare received a strategic investment from New Mountain Capital, LLC. This investment is noteworthy because it originates from a reputable, growth-focused firm that manages around USD 55 billion in assets. The partnership intends to enhance Access Healthcare's capabilities and support its expansion into new markets.
- In September 2024, CorroHealth, completed the acquisition of the Xtend healthcare revenue cycle management business from Navient. This strategic move is significant for several reasons, which will be explored in detail below. As part of this transaction, over 925 employees from Xtend have joined CorroHealth’s workforce. This addition not only expands CorroHealth’s team but also brings in valuable expertise that can enhance their operational capabilities.

No comments:
Post a Comment